Real-time monitoring system for textile membranes
Fabrics Sensor Technology Technical Textiles Smart Textiles Tests
Abstract
In the IGF project 01IF22600N, a real-time, fiber sensor-based monitoring system for textile membranes was developed at the ITM of TU Dresden. Textile membrane structures are used in numerous technical applications, but methods for continuous, full-area condition monitoring have been lacking until now. The project goal was to implement an integrated sensor system that detects the global stress state of the membrane and thus provides indications of overloads and damage. To this end, suitable thread-like sensor materials were identified, sensor structures were integrated into the membrane using embroidery and weaving techniques, and robust contacting and coating strategies were developed. Based on experimental data and FEM simulations, an AI-based regression model was developed that determines load positions in real time with an accuracy of ±3 mm and load amounts with ±0.6 N, and uses this information to derive the full-surface stress state. The results show that the mechanical performance of the membrane is largely maintained despite sensor integration and that textile structures can be effectively expanded into intelligent, self-monitoring support structures.
Report
Introduction
Textile membrane structures have established themselves as lightweight, flexible, and yet high-performance components in numerous technical applications, such as architectural roof and facade systems, mobile and stationary protective structures, and maritime environments. However, their load-bearing capacity and fatigue strength depend crucially on static and dynamic stresses, as local overloads and undetected damage can lead to sudden structural failure in extreme cases. In practice, inspections have so far been based predominantly on visual checks and selective measurements, which do not allow for continuous condition monitoring or comprehensive evaluation of membrane behavior and are therefore of limited value for predictive maintenance. Against this background, the IGF project 01IF22600N aims to transform textile membranes into intelligent, sensor-functionalized structures that record their own stress and damage status in real time. To this end, a textile sensor structure [1] is integrated into the membrane structure [2, 3] and its measured values are evaluated in combination with simulation results [4, 5] using AI-based algorithms [6].
Objective
The central goal of the project was to create a fiber sensor-based monitoring system that determines the full-surface stress distribution of textile membranes and can thus provide indications of fatigue and structural damage. To this end, thread-like sensor materials were examined for their elongation properties and suitability for use in combination with the membrane. Using the preferred variants, weaving patterns for fabrics with integrated sensor and energy supply structures were developed and manufactured. These patterns were mechanically characterized while simultaneously recording the sensor measurements. At the same time, the global strain distribution was simulated for the test scenarios. Based on this data, algorithms were developed that calculate the global strain distribution from the sensor measurements and output it in real time, e.g., as a heat map. The developed system was successfully implemented and integrated into a functional demonstrator.
Results
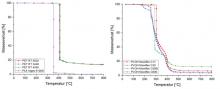
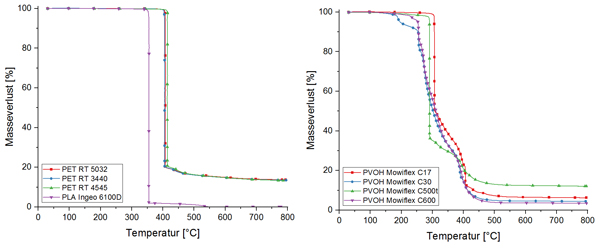
Thread-shaped sensor materials
Silver-coated polyamide yarns, pseudoelastic shape memory alloys (SMA), and precision resistance alloys were selected as promising options in the search for a suitable thread sensor material. The behavior of the electrical resistance under tension, the temperature stability, and the suitability for subsequent textile integration into the membrane composite were investigated. Cyclic tensile tests up to 10 % strain were chosen as the characterization method and were repeated at various temperatures between -20 °C and 70 °C. As a result of these investigations, SMAs proved unsuitable due to their high temperature dependence and strongly non-linear resistance behavior. Both precision resistance alloys (Isaohm® / Isabellenhütte) and silver-coated polyamide yarns (SilverTech+® 150 / Amann & Söhne GmbH & Co. KG) appeared to be fundamentally suitable and were taken into account in the following tests, with precision resistance alloys being identified as the preferred option due to their lower temperature dependence and linear sensor behavior. A fine wire (LitzWire / Rudolf Pack GmbH & Co. KG) was selected for the implementation of the electrical contact network due to its good textile processability and low basic electrical resistance (<< 1 Ω/m).
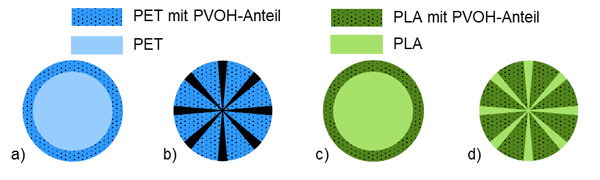
Development and production of functional samples
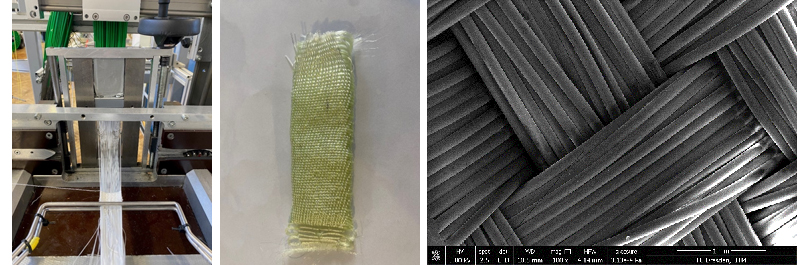
Two approaches were pursued for the development of a functional sample. On the one hand, samples were produced using embroidery technology and the TFP process; on the other hand, the thread-like sensor and the textile feed line were already integrated into the semi-finished textile product during the weaving process. For the embroidered samples, a commercially available membrane (HEYtex tentorium 900) was used. Both the silver-coated polyamide yarn and the precision resistance alloy were applied in patches using the tailored fiber placement (TFP) process (Figure 1) in order to increase the sensor length and thus improve measurement accuracy. In addition, the sensor patches were applied in different orientations in order to detect stretching in different directions. At the same time, the silver-coated polyamide yarn Shieldex® 117, which is more robust in textile processing than SilverTech+® 150, was embroidered using regular zigzag and chain stitches without auxiliary thread.
For the woven patterns, a grid with weft and warp threads made of feedline and sensor material was designed, which was combined with the polyester base fabric in terms of pattern (Figure 2). This made it possible to create arrangements with sensors in the warp and weft directions, which later allowed the calculation of tensile stress in different directions. A total of three patterns were created, which differed in terms of the length and position of the sensors. The third variant was a hybrid that combined a woven supply network with sensor patches that were embroidered on afterwards. Two types of intersection points, with and without electrical contact, were created in the conductive structures and implemented using binding techniques. The samples were produced on a gripper loom with center transfer (Lindauer Dornier P1).
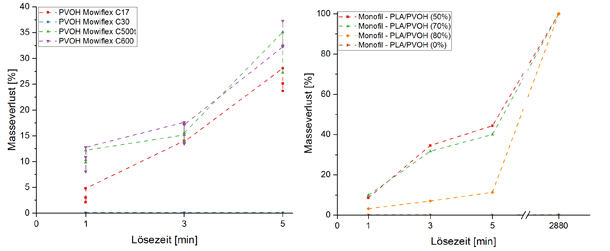
A key development step was the creation of practical contacting strategies for the sensor network. Conventional soldering methods caused damage to the textile base material due to high process temperatures, while alternative conductive adhesives initially exhibited excessive contact resistance in the kΩ range. However, by using an epoxy-silver conductive adhesive (8330S) with defined curing (160°C, 90 s, light pressure), stable, low-resistance contacts could be achieved both within the fabric and at the edges of the goods; in combination with crimp contacts, a mechanically robust and electrically reliable connection to external measurement technology was achieved.
Coating of the textile semi-finished product with integrated sensor structure
The functionalized fabrics were then coated with a PVC paste (plus 5% bonding agent) provided by the industry partner using a LineCoater from COATEMA (Figure 3). It was found that both integrally woven (0.2 mm) and embroidered sensor and supply structures (0.7 mm) could be integrated into the membrane with a low application thickness, so that the basic mechanical properties of the membrane were only minimally altered, while complete coverage and electrical insulation of the sensor technology was achieved. Additional tests with transfer foils and directly applied PVC adhesive layers showed that manual or semi-manual coating strategies are also suitable for local or subsequent functionalization, especially for smaller membrane areas.
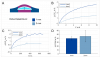
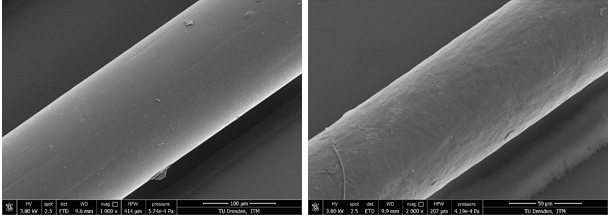
Characterization of the membrane with integrated sensor technology
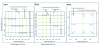
The manufactured samples were first tested in uniaxial tensile tests. In addition to the basic mechanical properties, the electromechanical properties were also determined. Particular attention was paid to the influence of the integrated sensor technology on structural integrity. Tests were carried out in both the weft and warp directions. With a maximum force of 3810 N at 23.2 % elongation in the weft direction and 4100 N at 24.9 % elongation in the warp direction, the manufactured samples were at a similar level to the commercial product from Heytex (weft: 3780 N at 25.8 %; warp: 3920 N at 20.6 %). Accordingly, it was not expected that the mechanical performance would be affected by the integration of the sensor network.
Development of algorithms for full-surface strain state detection
Based on biaxial tensile tests of the commercial membrane, FE models were created for the full-surface simulation of stress conditions. In addition to providing a database for algorithm development, this also supported the selection of suitable sensor layouts. The modeling was based on shell elements with an anisotropic material model. Based on the calibrated material model, simulations were performed with randomly varied load positions and magnitudes, which formed part of the database for algorithm development.
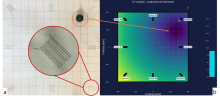
The AI model underlying the algorithms was based on a regressive model. To this end, the previously simulated load cases were applied to the demonstrator. The resulting sensor measurements were used to train the model. The model was then evaluated using the parameters mean absolute error (MAE), root mean squared error (RMSE), and coefficient of determination (R²). For the functional demonstrator, which consisted of a square, flat membrane, high accuracy was demonstrated for position determination in the single-digit mm range. The amount of load was also determined precisely with a coefficient of determination of 0.9604. The system achieves ± 3 mm spatial resolution and ± 0.6 N force accuracy for demonstrator loads < 50 N and is scalable up to kN load ranges. Based on the determined values for the position and magnitude of a load application, the corresponding full-area stress state was determined using multi-stage k-nearest neighbor models. The resulting model showed a high regression quality with a deviation of less than 5% from the FEM reference. In addition, the model proved to be very stable in general and allowed the desired real-time determination of the stress distribution. For the functional demonstrator, the results of the model were visualized in real time on a display unit next to the membrane (Figure 4), so that the effect of applied loads was immediately apparent to the user.
Conclusion
In summary, the IGF MeMo project shows that PVC-coated PES membranes can be further developed into intelligent, real-time capable support structures by combining suitable sensor materials, textile integration strategies, and robust contacting and coating processes. The experimental results prove that the mechanical performance of the membrane is largely retained despite the integration of the sensor technology and that the functional requirements – in particular with regard to the measuring range, temperature stability, and long-term behavior of the selected sensor materials – are met. The project developed an AI-based regression approach that determines load positions and amounts in real time from textile-integrated sensor signals and derives full-surface stress states from them without requiring numerical simulations during operation. The approach is characterized by high robustness against sensor-related scatter and low requirements for computing power and training data. The underlying methodology is fundamentally transferable to other large-area, deformable structures with integrated sensor technology, for example in textile architecture, lightweight construction, or membrane- and composite-based structural systems, e.g., in the maritime sector.
At the same time, the investigations clearly show that the type of integration and contacting has a significant influence on the quality of the sensor signals: Inline-contacted, integrally woven sensors are technologically sophisticated and currently still limited in terms of signal stability, while embroidered sensor networks with clearly defined, easily accessible contact points deliver significantly more robust and easier-to-evaluate signals. Thus, the work not only provides a complete technical toolkit, but also a clear preference for further system development towards embroidered, hybrid membrane solutions.
In the field of mechanical and electromechanical characterization, it seems sensible to expand biaxial testing programs on functionalized membranes. This would allow for an even closer link between experimental and numerical data and extend the validation of the material and damage descriptions used in the FEM models to the sensor membrane system as a whole. At the same time, the algorithms for load localization and stress reconstruction based on the data available to date can be expanded to include additional load collectives, more complex boundary conditions, and additional failure patterns, so that the monitoring system will continue to operate reliably in the long term, even in highly variable application scenarios.
On this basis, manufacturing and retrofitting concepts can be developed with a view to implementing intelligent, self-monitoring membrane structures in various industries - from construction and protective and safety applications to the maritime sector.
Acknowledgement
The IGF project 01IF22600N of the research association Forschungskuratorium Textil e.V., Reinhardtstr. 12-14, 10117 Berlin, was funded by the German Federal Ministry for Economic Affairs and Energy via the German Aerospace Center (DLR) as part of the program for the promotion of Industrial Collective Research (IGF) based on a resolution of the German Bundestag.
The authors would like to thank the aforementioned institutions for providing the financial resources. The research report and further information are available from the Institute of Textile Machinery and High Performance Material Technology at TU Dresden.
References
[1] J. Mersch, C. A. G. Cuaran, A. Vasilev, A. Nocke, C. Cherif, and G. Gerlach, "Stretchable and Compliant Textile Strain Sensors," IEEE Sensors J., vol. 21, no. 22, pp. 25632–25640, 2021, doi: 10.1109/JSEN.2021.3115973.
[2] K. Bremer, F. Weigand, Y. Zheng, L. S. Alwis, R. Helbig, and B. Roth, "Structural Health Monitoring Using Textile Reinforcement Structures with Integrated Optical Fiber Sensors," Sensors (Basel, Switzerland), vol. 17, no. 2, 2017, doi: 10.3390/s17020345.
[3] E. Haentzsche, R. Mueller, T. Ruder, A. Nocke, and C. Cherif, "Integrative Manufacturing of Textile-Based Sensors for Spatially Resolved Structural Health Monitoring Tasks of Large-Scaled Composite Components," MSF, 825-826, pp. 571–578, 2015, doi: 10.4028/www.scientific.net/MSF.825-826.571.
[4] T. D. Dinh et al., "A study of tension fabric membrane structures under in-plane loading: Nonlinear finite element analysis and validation," Composite Structures, vol. 128, pp. 10–20, 2015, doi: 10.1016/j.compstruct.2015.03.055.
[5] T. D. Dinh, A. Rezaei, L. de Laet, M. Mollaert, D. van Hemelrijck, and W. van Paepegem, "A new elasto-plastic material model for coated fabric," Engineering Structures, vol. 71, pp. 222–233, 2014, doi: 10.1016/j.engstruct.2014.04.027.
[6] J. Vitola, F. Pozo, D. A. Tibaduiza, and M. Anaya, "A Sensor Data Fusion System Based on k-Nearest Neighbor Pattern Classification for Structural Health Monitoring Applications," Sensors (Basel, Switzerland), vol. 17, no. 2, 2017, doi: 10.3390/s17020417.
Contact: hung.le_xuan@tu-dresden.de
Technische Universität Dresden
Fakultät Maschinenwesen
Institut für Textilmaschinen und Textile Hochleistungswerkstofftechnik (ITM)
01062 Dresden































![Abbildung 3: Zugfestigkeit (Fmax) der Multifilamentgarne aus Chitin gelöst mit EMIMOPr (links); Vergleich der Zugfestigkeiten der Chitinmultifilamentgarne mit Chitosanfasern aus Essigsäure-basiertem Nassspinnpro-zess [11] und mittels IL (EMIMOAc) hergestellten Chitosanfilamentgarnen [12] (rechts)](/sites/default/files/styles/thumbnail/public/2025-06/Abb3.png?itok=zmIRsVko)